- 1-833-448-3843 Make a call.
- info@givetouhf.ca Drop us an email.
- We are located in Edmonton, Alberta
Now showing, in 3D
The Servier Virtual Cardiac Centre allows doctors to see inside the heart

That’s the mission of the Servier Virtual Cardiac Centre (SVCC), so-named in recognition of a $1 million gift from Servier Canada to the University Hospital Foundation in support of advancing innovation in cardiac care at Alberta Health Services’ Mazankowski Alberta Heart Institute.
A team of doctors from the Mazankowski Alberta Heart Institute (Maz), researchers and scientists from the University of Alberta’s Faculty of Medicine and Dentistry and Faculty of Computer Sciences worked together to develop and implement 3D cardiac imaging – to the benefit of cardiac patients across western Canada, and beyond.
“We have the technical base to develop new knowledge right here in Edmonton that will be used around the world,” says Dr. Michelle Noga, Director of the SVCC, and cardiac radiologist at the Maz.
There’s plenty of innovation that this lab has embraced in its very short existence. Walk in, and you’ll see a couple of large screens and a bank of smaller computers. An image of a patient’s heart is called up on the largest screen, and Dr. Noga hands me a pair of 3D glasses. I put them on, and now the heart is floating in front of my eyes.
“It’s like comparing a 3D movie to a flat-screen TV,” she says.
But it’s not just about the doctors. A patient can view his or her own organs. Instead of receiving a diagnosis filled with Latin and complex medical terms, a person can look at his or her own heart and be shown what’s wrong.
“It helps the patient understand what’s happening in their own body,” says Noga. “They’ll better understand the surgery that’s coming up, they’ll understand what’s going to happen to them. And patients are all curious about what they look like on the inside.”
She shows a new example on the screen; with the glasses on, we see a 3D image of a heart valve. It opens, but there’s a gap when it’s supposed to close. She explains that this is an image from an infant who had a heart defect — a leaky valve. Without any medical training, I can see that the valve doesn’t close properly. Now, imagine the nervous parents of this child being shown this image; they’ll know exactly what the doctors have to do, and why.
A patient can view his or her own organs. Instead of receiving a diagnosis filled with Latin and complex medical terms, a person can look at his or her own heart and be shown what’s wrong.
This also helps with patients who might not be taking their medications or following their diets. We can be told that we have a heart condition, but we’ll feel fine and think that it’s OK to cheat on our diets or skip our pills. Using the 3D image, the patients can see that there are issues with their health that need to be constantly addressed. It works a lot better than a verbal diagnosis in passing on the message.
As Noga says, when a patient sees a scan, it’s a “eureka moment.”
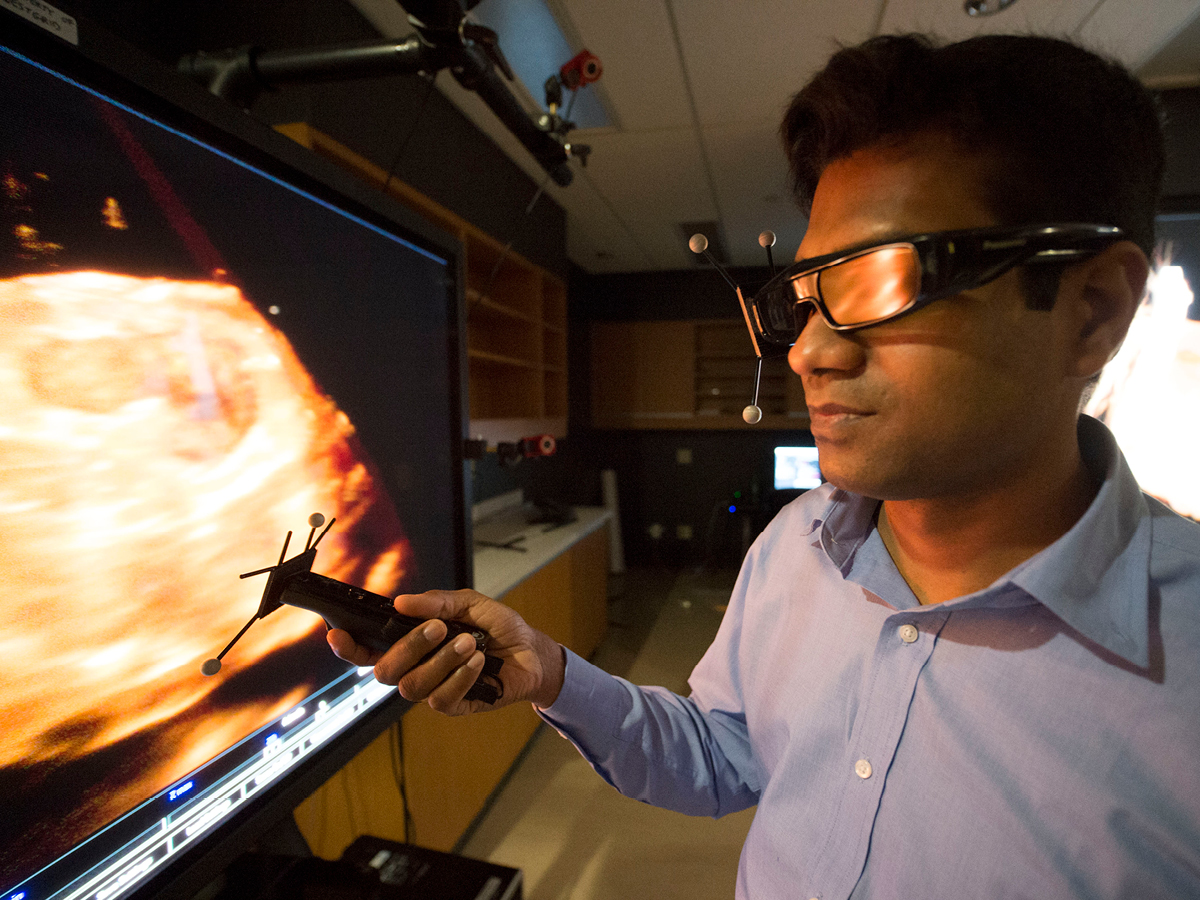
I’m given a headset with goggles attached, no different than the VR headsets you find at a Best Buy’s video-game section. I’m handed two controllers, one for each hand, that, well, feel exactly like I’m about to play the latest BioWare game. Using the triggers on the controllers, I can control the 3D image of the organ in front of me, I can even make cuts to it to look inside.
The images can be created by fusing ultrasound images together. And the images are so clear that doctors can possibly pick up things that might have been missed by traditional scans. It may be easier to see early signs of heart disease or cancer in high-risk candidates. And, of course, the earlier an abnormality is spotted, the easier it is to treat.
“As technology advances, so do our tools,” says Noga. “The technology just keeps getting better and more affordable.”
And that means, for cardiac patients at the Maz, even greater chances of recoveries and successful returns to their lives.
Partnering to make life better for Albertans
Through the University Hospital Foundation’s Strategic Partnerships program, innovative companies like Servier Canada, the Canadian arm of the international pharmaceutical company, Servier, team together with the Government of Alberta and UHF to form a unique collaboration called a public-private philanthropic partnership. Partnerships like this are able to tackle more complex global health issues — for the advancement and wellness for all Albertans and beyond.
In 2017, Servier upped its investment in patient care at the University of Alberta Hospital with the creation of the $1.7 Million Servier Alberta Innovation in Health Fund (SAIHF) in support of advancements in the cardiac sciences, diabetes, neurology and oncology.
