- 1-833-448-3843 Make a call.
- info@givetouhf.ca Drop us an email.
- We are located in Edmonton, Alberta
Brain Gain
Doctors at the University of Alberta Hospital have more tools than ever to take care of your brain.
In 1999, Health Canada approved the clot-busting drug known as tPA (tissue Plasminogen Activator) for use on stroke patients — an incredible breakthrough considering that, until then, there was no real treatment for strokes at all.
However, tPA came with conditions. It could only be used if doctors were sure that stroke symptoms began within four and a half hours of administering the drug, and only if the patient had first undergone a CT scan to determine the cause of the stroke. That’s because tPA was only effective on ischemic strokes — strokes caused by blood clots. Hemorrhagic strokes, caused by bleeding in the brain, cannot be treated with tPA.
At Alberta Health Services, the challenges that come with caring for the brain, combined with a desire to continually improve and provide leading edge care in the neuro-sciences program, led to the University Hospital Foundation’s Brain Centre Campaign. A remarkable $60 million in community donations has proven to be a catalyst for innovative, out-of-the-box thinking, and the evolution to one of the one of the top brain centres in North America.
With world class neurologists, neurosurgeons and specialized care teams, supported by incredible diagnostic imaging, and various options to treat complex brain conditions including strokes, tumours, epilepsy, Parkinson’s, brain injuries and more, the University of Alberta Hospital is the centre for brain care in Western Canada.
The University Hospital Foundation’s Brain Centre Campaign received $60 million in community donations which has been a catalyst for innovative, out-of-the-box thinking.
Clot busters
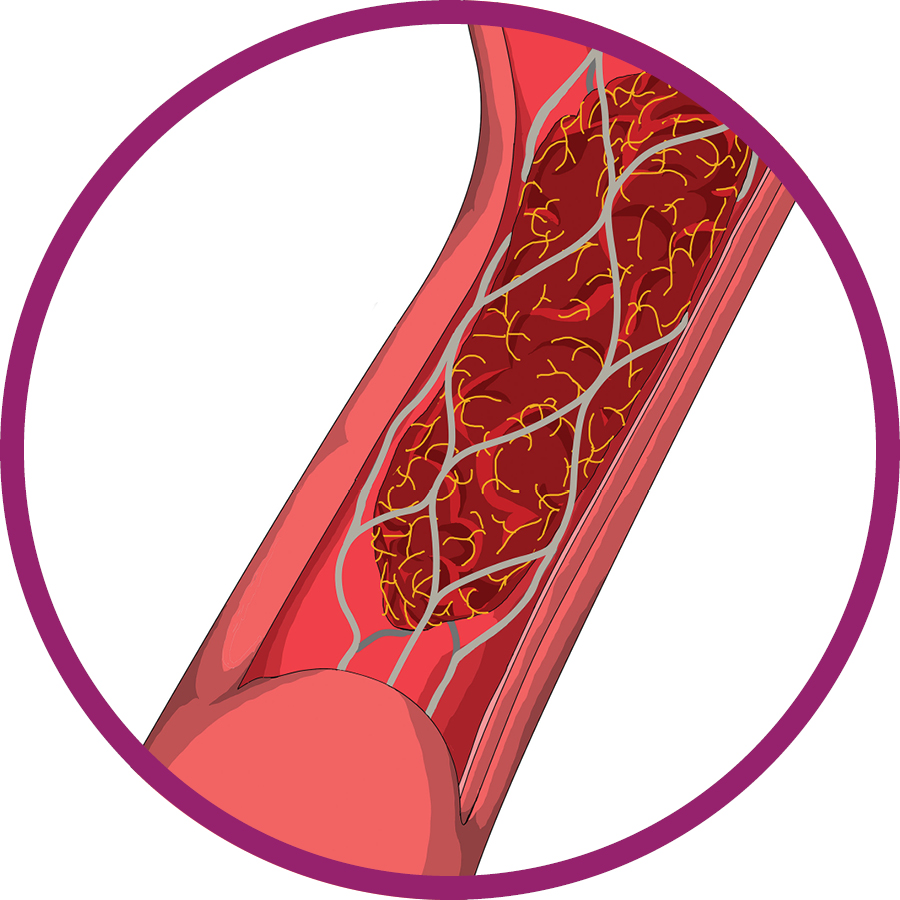
With a clot retrieval procedure known as Endovascular Thrombectomy (EVT), Interventional Neuroradiologists at the University Hosptial like Dr. Jeremy Rempel can save even more lives of stroke patients. “It’s the most significant development in stroke care since tPA,” he says.
Starting with an incision in the patient’s groin, Rempel passes a tiny catheter up to the brain and deploys a small stent. (No, he does not use Siri to find his way.) The procedure is performed using a medical imaging device called Biplane Angiography that provides crystal clear, real-time images of our veins and arteries. With a large flat-panel television- like screen in front of him, Rempel follows a literal pathway to the brain and is able to locate, and remove, the offending clot. Blood flow is immediately restored.
To date, the procedure has cut mortality rates in half for patients who receive stroke treatments. and significantly increases the chances of returning to a normal lives.
“It’s the most significant development in stroke care since TPA.” – Dr. Jeremy Rempel
The knife that doesn’t cut
When Major Steve Kuervers, Battery Commander at 20th Field Regiment, Royal Canadian Artillery in Edmonton, was told he had a brain tumour, the silver lining was that as long as it didn’t grow, he’d be fine.
A year later, it started to grow. Kuervers envisioned open brain surgery. Three months in hospital to recover. His career? He didn’t want to think about it. His family? Let’s just take this one step at a time.
Instead, he had Gamma Knife radiosurgery. The most advanced form of non-invasive brain surgery in the world, Gamma Knife uses up to 192 precisely aimed beams of radiation. After beng funded with $17.2 million in donations to the University Hospital Foundation, including $3 million from the Scott and Brown families, the Gamma Knife has been in use at since 2017. Hundreds of brain patients, with conditions that include growths, malformations and metastatic cancers that have spread to their brains, have benefitted from the treatment. It has literally transformed brain surgery into day surgery.
In Kuervers’s case, he was home in time to take his dog for a walk the same day he had his surgery.
Magnet medicine
 Dr. Keith Aronyk, neurosurgeon at the University of Alberta Hospital, says the surgeons who visit the hospital from all over the world marvel at what they call one of the most advanced surgical suites they’ve ever seen.
Dr. Keith Aronyk, neurosurgeon at the University of Alberta Hospital, says the surgeons who visit the hospital from all over the world marvel at what they call one of the most advanced surgical suites they’ve ever seen.
It’s officially called the Dan and Bunny Widney Intraoperative MRI Surgical Suite, in honour of that couple’s generous donation, and what’s inside is a larger-than-usual operating room with spectacular technology to help surgeons see deep brain structures like never before — a good thing when it comes to brain surgery.
But the real majesty of the suite arrives when the surgical team steps back to assess its work, and determine next steps. Typically, this would involve wheeling the patient out of the operating room to the closest MRI (Magnetic Resonance Imaging) unit. Shaped like a giant doughnut, the superconducting electromagnet weighs upwards of six tonnes. It is used to create spectacular images by sending radiofrequency waves through the brain at all angles, while under the influence of a powerful magnetic field.
In the intraoperative suite, two large steel doors slide open, and an MRI enters via a track mounted to the ceiling.
Images of the patient are taken immediately. If more surgery is required, it happens in the moment, sparing the patient the anxiety of waiting for results — and another surgery.
